The first signs of cervical osteochondrosis are quite difficult to notice. Often they cause so little discomfort that a person does not pay attention to them and does not rush to consult a doctor. In other cases, the symptoms are confused with simple fatigue or a mild flu:
- increasing pain in the neck;
- heaviness in the back of the head;
- slight tingling in the hands.
These signs appear in thousands of people every day, but only a few can recognize them as cervical osteochondrosis.
Important! Remember that the disease develops slowly, and in the first stage it is easier to resist the development of the destructive process than to treat the advanced stage!
Who is at risk?
Osteochondrosis develops not only in those who lead a sedentary life. Athletes from fields such as classical wrestling, judo, freestyle wrestling, and sambo also suffer from this disease. The disease develops due to the critical load on the spine in the cervical region (falls and constant blows, high mobility of the neck). It is important to consider that osteochondrosis is often diagnosed before the age of 35 - more than 86% of cases.
How the disease develops
Currently, osteochondrosis of the cervical spine is more common than other pathologies of the spine. This is due to greater neck movement. As the disease progresses, severe pain appears, which worsens a person's life. Osteochondrosis develops slowly, but definitely leads to degenerative changes in the bone tissue of the spine. There are four stages of disease progression:
- The first stage is characterized by an almost complete absence of symptoms. This disease can only be diagnosed during a routine examination. Sometimes mild pain may occur, which many identify as a sign of stress or fatigue. In the first stage, the destruction of the nucleus pulposus occurs, because of this the vertebrae begin to bear more severe loads. As a result, the degenerative-dystrophic process develops. Among the first symptoms are: mild headache that quickly disappears, cramp syndrome "in the neck", significant muscle tension in the upper back.
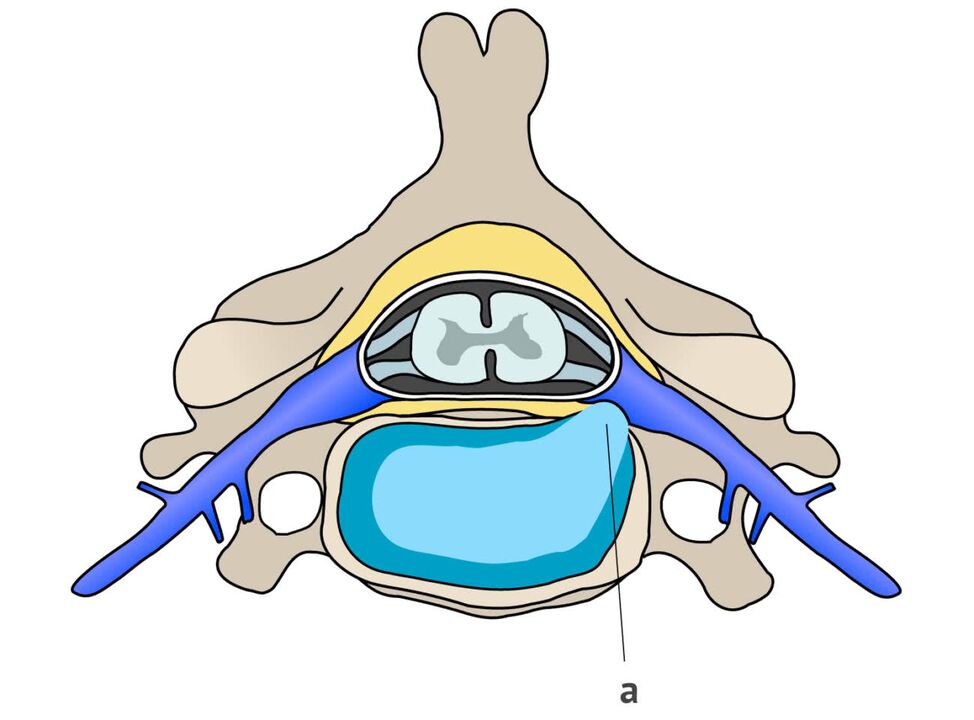
- In the second stage of the disease, cracks appear on the side of the disc due to pressure. They are not yet very deep, but they already contribute to squeezing the nucleus. During diagnosis, protrusion is often detected and the height of the disc decreases. This stage is characterized by frequent and prolonged pain. A person loses strength, certain areas of his face begin to go numb, and stiffness of movement develops due to fear of new pain sensations.
- The third stage is characterized by the formation of a hernia in the cervical region between the vertebrae. All tissues along with vessels located in this area - veins, muscles, nerves, arteries - are also affected. The pain flows smoothly and spreads from the neck to the occipital region. Certain sensitivity occurs when moving the head. The patient also began to complain of dizziness due to insufficient blood flow in the vertebral artery.
- In the fourth stage, osteophytes are formed - bone tissue grows in width because the body and brain literally send a signal that requires an increase in area to distribute the load. As a result, the vertebral nerves are pinched, the cavity between the vertebrae decreases, severe stiffness occurs, and sometimes the impossibility of movement. All adjacent joints are damaged. To eliminate the cause and "contain" cervical osteochondrosis at this stage, it is necessary to carry out long-term and difficult treatment, including surgical intervention.
Prevention of cervical osteochondrosis is an important process that will help stop the deterioration of the cervical vertebrae, relieve complications and preserve your quality of life. But to identify the pathology, you need not only to monitor the symptoms, but at least once a year to carry out diagnostics and take the necessary tests.
Symptoms of cervical osteochondrosis
Even small changes in the vertebrae, ligaments and intervertebral discs lead to disruption of the function of the nerve endings. Blood vessels are also affected. All of them connect directly to the brain and other organs, where unpleasant symptoms arise.
Important! It is the compression of blood vessels and nerves that leads to severe discomfort and pain.
Clinical symptoms of cervical osteochondrosis are divided into three groups:
- the first group is characterized by pathological neurological manifestations that arise as a result of the effects of the inflammatory process and changes that occur in the tissues of the peripheral part of the nervous system;
- the second group is associated with the effects of processes on the spinal cord;
- The third group includes signs that depend on the disruption of processes in the nerve endings leading to the brain.
As soon as a disturbance occurs in the peripheral nervous system, a person begins to experience pain. They don't always start suddenly and last for a long time, but they all start from the same place - inside the neck. Pain is not the same as muscle pain; when kneading, no slack.
In most cases, when the peripheral system is damaged, a feeling of shortness of breath occurs. Patients feel as if they have a "lump" in their throat and it becomes difficult to breathe. The pain is characterized as unexpressed, dull, and constant tension in the muscles is felt. Sometimes after sleeping overnight the pain increases.
The progression of the disease leads to the spread of symptoms. Following the head and neck, the arms begin to suffer:
- feeling weak;
- numbness occurs in one or more fingers;
- then the large part of the hand becomes numb.
If you feel pain and pressure in the heart area, you can talk about the development of cervicothoracic osteochondrosis. Osteochondrosis is often mistakenly identified as angina or neuralgia. It is mainly characterized by symptoms such as:
- cough;
- stomachache;
- discomfort in the heart;
- pain in the lungs.
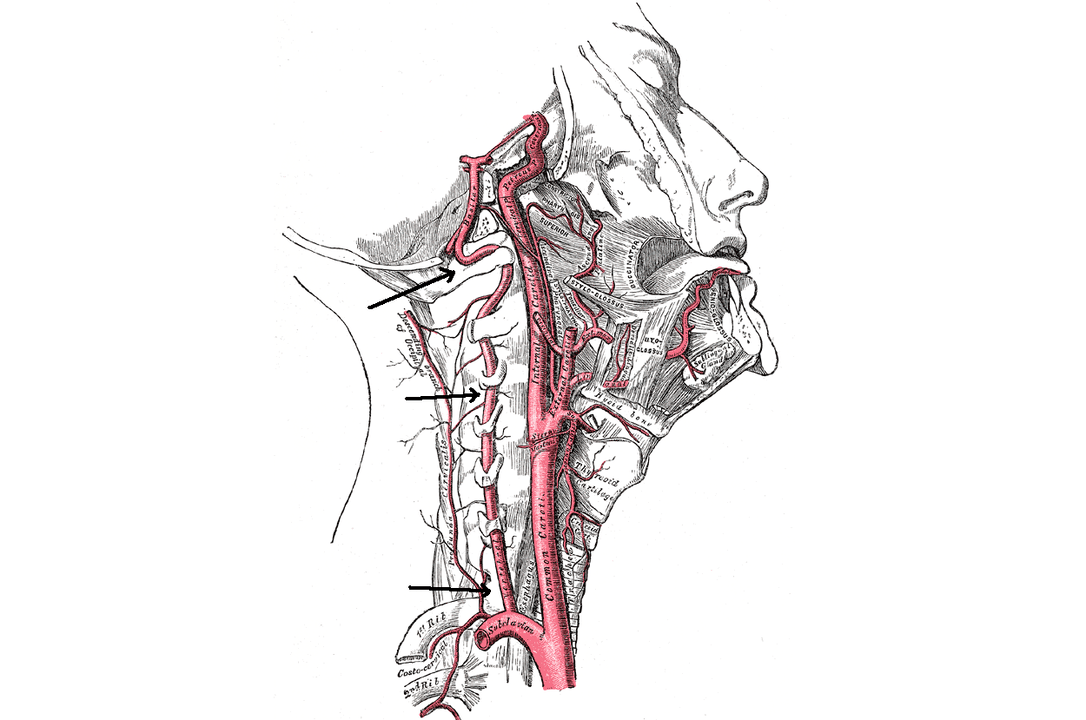
As soon as the vertebral artery is connected to the destructive process (it supplies the brain with oxygen), symptoms from the brain begin to appear. As the disease progresses, it becomes stuck and cannot function normally. This is how dizziness develops, vision deteriorates, and tinnitus occurs.
The use of conventional painkillers rarely helps with headaches with cervical osteochondrosis.
Physical activity and frequent nervous tension can trigger the severity of the pathology. Symptoms of worsening cervical osteochondrosis:
- increase irritability;
- sensitive and fleeting sleep;
- quickly tired.
If a person is diagnosed with vegetative-vascular dystonia, then the symptoms increase: neurosis develops, blood pressure rises. The diagnosis may also indicate the development of cervical osteochondrosis, so it is necessary to pass all the tests, undergo an MRI and take other pictures of the cervical spine.
It is almost impossible to independently diagnose cervical osteochondrosis based on symptoms. Since the first stage occurs without obvious signs, it is necessary to undergo regular preventive examinations. At the first signs of the disease, treatment should begin, according to the doctor's recommendations. Although the disease has not "played" and does not cause significant problems.
Syndrome
For an accurate diagnosis of cervical osteochondrosis, proper symptom justification is required. Based on tests, images and examinations, the doctor must determine the exact cause of the symptoms. All of them are associated with certain syndromes.
Humeroscapular periarthritis
This syndrome is characterized by severe pain and muscle contracture in the area of one of the shoulder joints. In left-handed people, the left shoulder joint is usually affected, and in right-handed people, the right joint is affected. Features of the pain syndrome:
- constant;
- sick;
- heartache
In most cases, the pain increases at night. If you move your hand to the side or put it behind your back, the pain will also increase. Sometimes the pain is felt throughout the arm, in the occipital and scapular region.
During the examination, the doctor often sees tension in the joint area, and during palpation the patient feels severe pain in the muscles. In some cases, doctors notice compaction and small nodules during palpation, and there is slight swelling of the affected shoulder.
Radicular syndrome
This syndrome can develop when the spinal roots are damaged. It usually appears several years after the onset of osteochondrosis. Irreversible destruction occurs in the vertebrae and discs: the cavity consisting of nerves and vessels decreases, when the cartilage becomes thinner or intervertebral hernia forms. Osteochondrosis with radicular syndrome is characterized by certain symptoms:
- pain is observed in the forearm, in the shoulder blade area, and moves to the front of the chest;
- it becomes difficult to move the neck, pain and stiffness are felt;
- The sensitivity of the skin on the hands worsens, it becomes numb, and a feeling of "goosebumps" appears;
- one cannot raise his hand from the side of the affected part.
Irritation-reflex syndrome
This syndrome is characterized by a rather burning and sharp pain in the back of the head and neck. It appears when you move your head after a long period of immobility, for example, while working at the computer. Discomfort is felt in the shoulder joints, as well as in the chest area.
Cardiac syndrome
This syndrome is often confused with angina pectoris, because the symptoms of the disease are almost the same. This happens because the pain and contraction of the muscle tissue in the heart area occurs due to the compression of the root in the lower part of the cervical spine. Hence the disease equation.
This syndrome is characterized by pain that comes in attacks and can last from 10-15 minutes to several hours. Significantly aggravated by sudden movement (turning, coughing, sneezing). Often the cardinal syndrome is characterized by the development of tachycardia, and coronary dilators do not cope with the pain. There are also no signs on the cardiogram that are characteristic of circulatory disorders.
Vertebral artery syndrome
The role of the vertebral artery is to supply the brain and spinal cord. With this syndrome, the work of the periarterial sympathetic plexus is disrupted. The picture of the syndrome looks like this:
- headaches of varying intensity;
- disorders of the vestibular apparatus (shock, loss of balance);
- mild and severe dizziness;
- nausea vomiting;
- pharyngolaryngeal and ocular symptoms (deterioration of vision, the appearance of veils in front of the eyes).
With vertebral artery syndrome, burning pain often occurs not only in the neck, but also in the back of the head. Feelings of lethargy, resentment, and irritation develop. Anxiety levels increase, sleep and memory may be disturbed.
Therefore, to make an accurate diagnosis, it is necessary to determine which syndrome underlies cervical osteochondrosis. Based on certain symptoms, test results, pictures and palpation, an experienced doctor will be able to accurately determine the pathological features and prescribe the correct treatment.



















